What is a biofilms?
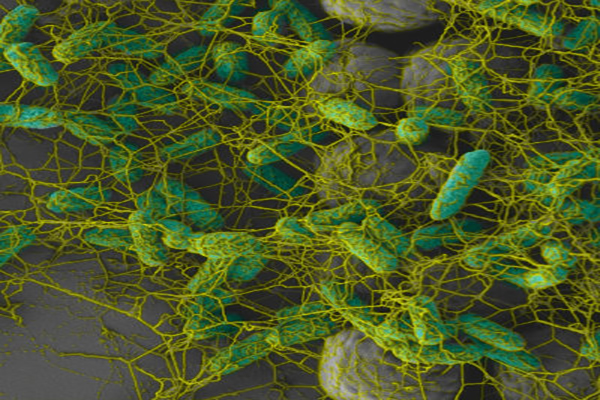
Many bacteria can form biofilms when finding a suitable surface on which to accumulate and grow. They are found on most surfaces, not only those subject to moisture. Even in a regularly cleaned hospital environment, these microscopic structures have proven to be present.
Despite routine cleaning in wards and ICU, dry surface biofilms have been found to be a significant contaminant. Because of their resistance to standard cleaning practices, and the fact that they are known to shelter antibiotic-resistant super-bugs, biofilms are a significant risk if not eliminated.
To effectively remove this threat, biofilms need to be broken up, removed and all pathogens inside them neutralised: all at the same time.
Why do biofilms form?
Planktonic, or free-floating bacteria are unattached to a surface and are able to spread through built environments. When it meets a suitable surface, bacteria begins to put down roots to ‘build a home’. To protect itself, it starts to exude a natural polymer made of carbohydrates & sugars. This substance then hardens to form a shelter for the bacteria.
These bacteria are biologically inactive until surrounding conditions become favourable for growth. If the surface remains dry for extended periods of time, the bacteria does not dry out and die, it simply waits for conditions to change. A small amount of moisture or food can trigger activity. Although bacteria are microscopic, they are smart and equipped to survive.
How do bacterial colonies grow?
Once bacteria creates the biofilm and the environment supports its growth, it will continue to exude more of the natural polymer, which can attract other bacteria. In addition, a “quorum sensing” technique sends out signals to nearby microorganisms as an invitation to “come join us”. This could include MRSA, VRE or COVID-19 to name a few.
As more and more bacteria respond, they create their own biofilms forming a community, a “city of microbes”. And once inside a biofilm, a bacteria will change its behaviour, which can render them up to a thousand times less susceptible to common disinfectants.
Previously, it was thought that bacteria needed moist conditions to survive, and dry environments would naturally kill off the microorganisms as it dried out. However, this has proven to be untrue. Surfaces do not need to be wet to provide suitable conditions for biofilms. When bacteria land on dry surfaces, they put out the biofilm and wait. These are known as dry biofilms, dry area biofilms, or dehydrated biofilms.
Can you spread dry biofilms?
Cross contamination of surfaces in healthcare plays a major role in the spread of dry surface biofilms. They exist on highly touched surfaces that pose a risk to patients and transmission by nitrile, latex, and surgical gloves is common.
When a biofilm matures, or becomes enlarged, it ruptures, releasing millions of bacteria & other microorganisms. Once these are released, they become free-floating and can land on a surface to start the whole cycle again.
In any built environment, this can explain why biofilms are present on a surface. And to make matters worse, if an infected surface is cleaned with a neutral detergent or with reusable cloths, transmission & contamination of new locations can occur, and biofilms can setup a new home once again. This causes the spread of bacteria regardless of whether the surface is wet or dry.
Why are dry surface biofilms hard to eliminate?
Because dry biofilms have been largely overlooked in the formulation of cleaning agents and disinfectants, there are very few commonly available products that are effective against them.
Careful attention should be paid to choosing a suitable surface wipe or disinfectant that can destroy a biofilm structure in a realistic timeframe (1-3 minutes) and kill all of the micro-organisms contained in it. Standard chlorine solutions and commonly used benzalkonium chloride products have little effect on dry surface biofilms.
“Anti-Biofilm” wipes and detergents that claim to have undergone testing at a medical facility or research centre without mentioning approved test methods, are also likely to be ineffectual in eliminating dry biofilms. Look specifically for ASTM test E2871-19, as this is the only currently recognised test approved of by the US EPA to indicate effectiveness against biofilms in life-like conditions.